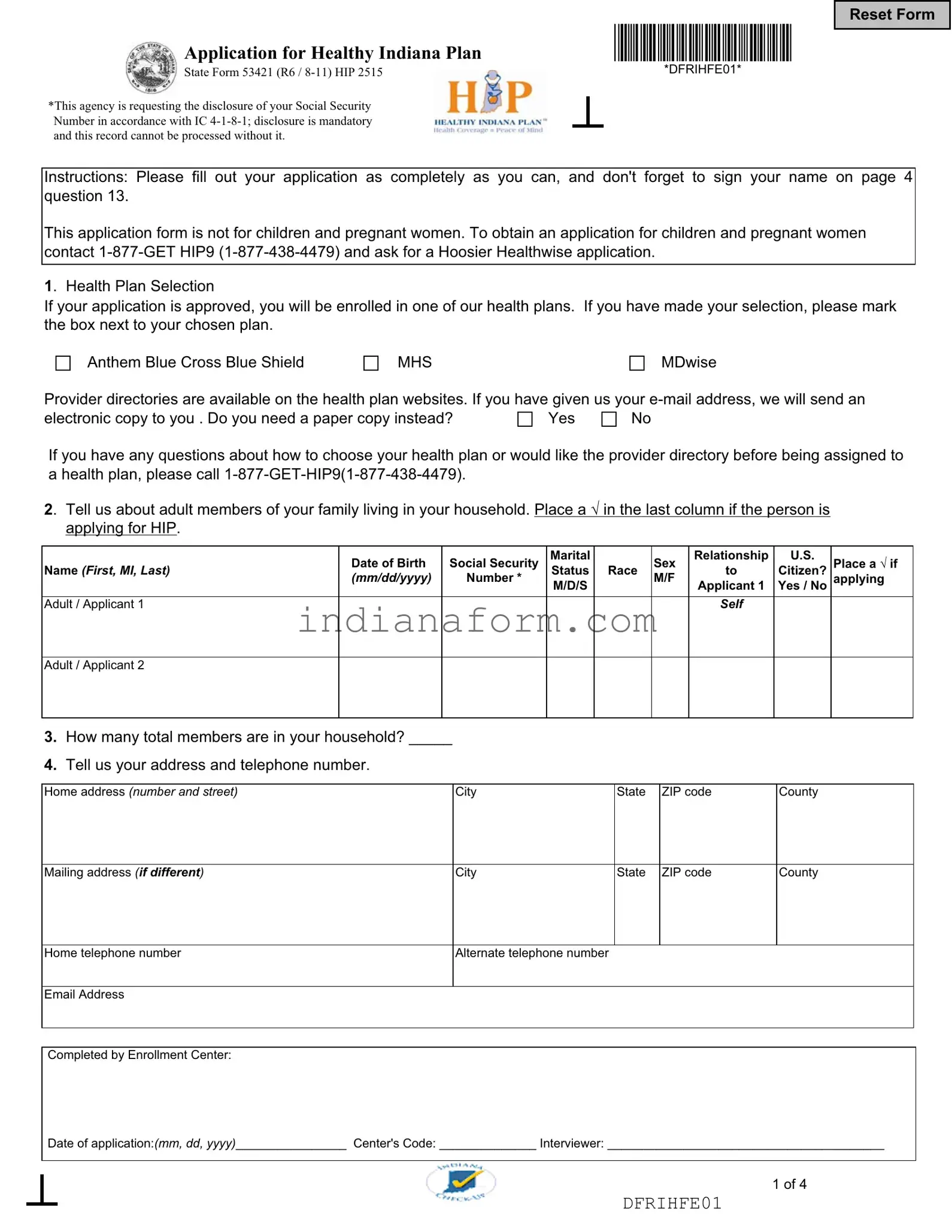
What is the Indiana 53421 form?
The Indiana 53421 form, also known as the Application for Healthy Indiana Plan (HIP), is a document for individuals seeking health coverage under Indiana's HIP program, designed for uninsured adults aged 19 through 64. The form requests comprehensive information to assess eligibility, including personal details, income, health conditions, and citizenship or immigration status.
Who needs to fill out the Indiana 53421 form?
Uninsured Indiana residents between the ages of 19 and 64 who are interested in applying for the Healthy Indiana Plan need to complete the Indiana 53421 form. It's important to note that this application is not intended for children and pregnant women, who have separate forms for different programs.
Why is my Social Security Number required on the form?
Disclosing your Social Security Number (SSN) on the Indiana 53421 form is mandatory as per IC 4-1-8-1. Without this information, the processing of your application cannot be completed. The request for your SSN is made to ensure accuracy in identifying your records and facilitating the assessment of your eligibility for the program.
Can I choose my health plan while applying for HIP?
Yes, upon approval of your application, you will be enrolled in one of the health plans offered through HIP. You have the option to select your preferred health plan from the choices provided on the form, such as Anthem Blue Cross Blue Shield, MHS, and MDwise. If you have specific preferences, it's important to mark your choice on the application.
What if I need a provider directory?
If you request a provider directory before being assigned to a healthcare plan, it can be sent to you electronically if you've provided an email address, or a paper copy can be requested. Provider directories help you understand the network of healthcare providers included in each plan.
Is information about household members necessary for the application?
Yes, the application requests details about adult members of your household, including their relationship to you, marital status, race, citizenship status, and more. This information is crucial for determining eligibility based on household size and income among other factors.
What should I do if I need help filling out the form?
If you need assistance completing the application or have questions about the Healthy Indiana Plan, you can contact customer service at 1-877-GET-HIP9 (1-877-438-4479). Support staff can provide guidance and answer any questions you may have about the application process or eligibility criteria.
What happens after I submit my application?
After submission, your application will be reviewed to determine your eligibility for the Healthy Indiana Plan. You may be contacted for additional information or documentation. Timely response to these requests is crucial for the processing of your application. Once reviewed, you will be notified of the decision and next steps for enrolling in a health plan.